Plantar Fasciitis
What is Plantar Fasciitis?

Bottom of foot region.
Plantar fasciitis is a painful inflammation of the thick band of tissue—known as the plantar fascia—that extends from the heel to the toes and helps to support the arch. The plantar fascia runs along the bottom of the foot like a rubber band, connecting the ankle to the toes. Under pressure from certain daily and athletic activities, the fascia becomes irritated and then inflamed, resulting in heel pain. When the fascia is overloaded or overstretched, it can cause small tears in the delicate tissue, especially where the ligament meets the heel bone.
Facts About Plantar Fasciitis
PLANTAR FASCIITIS FACTS:
- Heel pain is the most common problem affecting the foot, and the main cause of heel pain is plantar fasciitis.
- One in 10 people will likely develop plantar fasciitis during their lifetime,
- Plantar fasciitis affects about two million people every year.
- Plantar fasciitis is most common in young athletes (more male than female) and overweight middle-aged adults (more female than male).
Who Suffers from Plantar Fasciitis?
WHO SUFFERS FROM PLANTAR FASCIITIS?
Plantar fasciitis is common among people whose jobs require being on one’s feet for long hours at a time such as servers or nurses. Standing and walking on hard, flat surfaces like cement or hardwood puts abnormal strain on the plantar fascia and can cause or aggravate plantar fasciitis. People who are overweight or obese—especially women—have problems with their arches (either flat feet or high arches), or have trouble with ankle flexibility are also prone to developing plantar fasciitis.
If you’re a runner, play tennis on hard courts, or do any other running or jumping exercise on hard surfaces, you are also at high risk, especially if you have tight calf muscles that limit how far you can flex your ankles. The most common source of heel pain in athletes, plantar fasciitis affects runners in particular. The jumping and repetitive pushing off that accompanies running, especially on hard, paved surfaces, can easily cause an injury to the fascia such as a partial or complete tear of the ligament, and the surrounding tissue on the bottom of the foot. The damage to this tissue caused by plantar fasciitis can be a major disruption to an athlete’s training and routine. More importantly, it is extremely painful.
Symptoms of Plantar Fasciitis
SYMPTOMS OF PLANTAR FASCIITIS ARE:
- Pain on the bottom of the foot centered under your heel.
- Pain in the arch of the foot that radiates to the ball of the foot.
- Pain that is often at its worst first thing in the morning, especially the first step when you get out of bed.
- Pain is only temporarily relieved by resting.
- Pain that decreases after moving or walking, but returns after a prolonged time of standing, walking, or running
- Pain that may be mild at first, but gradually worsen over weeks or months.
What Causes Plantar Fasciitis?
Plantar fasciitis occurs when the fascia—the ligament running along the arch from the heel to the toes—is strained over time. This causes the soft tissue fibers to tear or stretch at points along its length, which results in the heel pain and stiffness of plantar fasciitis. Too much pressure on the delicate tendons and ligaments of the foot can damage or tear the tissue. The causes of this pressure include:
- Wearing shoes with poor arch support and shock absorption, especially
- old and worn running shoes
- high heels
- shoes with little or no padding or arch support
- Recent weight gain and obesity
- Being on your feet for extended hours
- Exercise that entails jumping or running on hard surfaces.
PLANTAR FASCIITIS INFLAMMATION
The body’s natural response to injury is inflammation, and your feet are no exception. All the things that can cause plantar fasciitis in the first place can aggravate the inflammation. The pain associated with inflammation usually develops over time and ranges from dull and throbbing to sharp and burning. It’s important not to ignore these early signs of plantar fasciitis, as the condition can get much worse if ignored.
Plantar fasciitis can also be caused or made worse by other foot conditions such as metatarsalgia or ball of foot pain that put a strain on the plantar tissues. And plain old wear and tear on your feet and heels as you age can also lead to plantar fasciitis.
The term plantar fasciitis covers both fascia inflammation due to ligament injury from physical activities and the degeneration of the fascia due to fat pad atrophy. In either case, the fascia becomes so thickened and taut when inflamed that it causes extreme pain from the bottom of the heel to the toes.
PLANTAR FAT PAD ATROPHY
Plantar fat pads are made up of little honeycomb walls filled with fat that act as shock absorbers under the calcaneus or heel bone to protect the underlying connective tissues, ligaments, and tendons. Unfortunately, plantar fat pads thin out over time and their shock-absorbing cushioning wears out—or atrophies. Thinner fat pads increase pressure, which can lead to pain under the heel and sole of the foot.
Hormone changes put women at increased risk of pain and disability from fat pad atrophy. Other conditions associated with fat pad atrophy include diabetes, rheumatoid arthritis, trauma, and chronic steroid use.
Resting, icing, and taking ibuprofen can help relieve the pain of fat pad atrophy. A heel lift insert can transfer some of your weight to the front of your foot, relieving pressure on your heel. Try walking or running on a soft surface, such as grass or a track instead of pavement, and wear slippers with good padding on hardwood or tile floors at home
EXCESSIVE PRONATION
In normal walking or running, your foot should pronate properly. You should land on the ground heel-first, then shift the foot—shifting your weight with it—to the outside of your foot, gradually rolling to the inside, the arch lining up with the big toe. This natural step motion provides flexibility and shock absorption. However, when you over-pronate, moving too much to the inside of your foot, you apply too much pressure to the arch, creating abnormal stretching and pulling on the plantar tissue from your arch to your heel bone. This can cause plantar fasciitis. Athletes in general and runners in particular can over-pronate when they run in worn or improperly fitted shoes. Wear running shoes with the proper arch and heel support for your foot, and buy a fresh pair of shoes every six months or so. People with flat feet can also be at risk for over-pronation and therefore plantar fasciitis.
OTHER TYPES OF HEEL PAIN OFTEN CONFUSED WITH PLANTAR FASCIITIS
- Bursitis is an inflamed bursa—a small fluid-filled sac between the tendon and bone—or swelling caused by the enlargement of the calcaneal bursa under the heel. Bursitis is very painful and develops from running too much or wearing shoes that rub or cut into the back of the heel. Bursitis can also be caused by thinning fat pads.
- Haglund’s deformity is a noticeable bump or bone enlargement at the back of the heel bone that often leads to bursitis. It’s also known as a “pump bump” because women’s pumps and other rigid shoes cause extreme rubbing and cutting against the back of the shoe that irritates the tendon and surrounding tissue.
- Rheumatoid arthritis is an inflammatory condition that affects the lining of your joints, causing pain and swelling. Swollen RA nodules can form on the heel bone, toe bones, or bottom of the foot, causing pain when they rub against shoes or when walking.
- Gout is another kind of arthritis that causes painful and stiff joints. Caused by the buildup of uric acid crystals in your joints, it often starts in the big toe, but can affect any joint, including the ankle and heel.
- Stone or bone bruise is a painful inflammation of the tissues that cover the heel bone, caused by stepping on a hard object such as a rock or stone that bruises the fat pad under your heel.
Preventing Plantar Fasciitis
Plantar fasciitis happens in large part due to overuse of the tissue and tendons running across the arch of the foot. It tends to affect active adults between 35 and 65 who are on their feet a lot. Being overweight also makes you susceptible as the extra pounds add more force or pressure to impact activities. And as we age, the fat pads on our feet thin and the tissue itself becomes less elastic, less able to be used without incident.
As a result, you want to do all you can to prevent plantar fasciitis from occurring in the first place. Maintain a healthy weight, make sure you do stretches and warm up before exercising or playing sports, and buy shoes that fit properly with good arch support and heel cushioning. Use orthotic inserts for extra support and padding in the arch or heel.
TIPS ON HOW TO PREVENT PLANTAR FASCIITIS
- Tape or strap your foot, taking pressure off of strained tendons and supporting the arch.
- Wear athletic shoes that fit well and have shock-absorbent soles, arch support, and heel cushions.
- Wear the proper shoe for what you’re doing: running shoes for running, tennis shoes for tennis, hiking boots for hiking. And good shoes for work: for example, low heels or wedges if you’ll be standing for long hours or walking a lot throughout the day.
- If the heels or soles of your shoes are worn down, replace your shoes. Who doesn’t want new shoes?
- Wrap ice in towel or fill a bag with ice and apply to the bottom of your heel for 10 or 20 minutes, before and after running, walking, or being on your feet for a long time.
- Rest your feet or foot, keeping it elevated on a pillow or ottoman.
- Don’t try and do ten miles the first time you start running. Build up your routine gradually.
- Warm up and do stretching exercises before and after exercising. Avoid walking barefoot on hard surfaces.
How to Treat Plantar Fasciitis
Once a diagnosis has been made, and treatment begun, most people with plantar fasciitis find pain relief in about two months, though it may take longer—six months to a year—for symptoms to resolve completely. Though treatment works in the majority of cases, many people can have pain for even longer. Those who have had plantar fasciitis are more likely to get it again. If you’ve suffered from plantar fasciitis before, you’ll want to do daily stretches and exercises to strengthen your feet and legs.
WHAT HELPS RELIEVE PLANTAR FASCIITIS PAIN?
Relieving the pain of plantar fasciitis includes resting and icing the foot, taking anti-inflammatories, and doing foot and ankle strengthening and stretching exercises. Massaging and stretching your feet and calves relieves pain as well as helping to lengthen the muscles and ligaments. Though pain is felt under the heel, the entire area from the calf to the arch is where treatment should be focused. In addition to stretching, try keeping weight off your foot as much as possible until the initial inflammation goes away. Icing your sore heel a few times a day may also relieve your symptoms.
FURTHER TREATMENTS FOR PLANTAR FASCIITIS
If your plantar fasciitis pain does not improve with home treatments, your doctor may prescribe physical therapy, steroid injections, or a night splint. Surgery is rarely in order for plantar fasciitis.
- Cortisone Injections. Cortisone is a steroid with anti-inflammatory properties that is injected into the plantar fascia to reduce inflammation and pain by decreasing plantar fascia thickness. Results can be seen in two weeks to a month following treatment. However, the effectiveness of cortisone injections does not typically last more than six months and multiple steroid injections can actually cause the plantar fascia to rupture, leading to a flat feet and other problems that cause chronic pain.
- Night Splints. Wearing a night splint keeps the plantar fascia in a neutral or slightly flexed position while sleeping. This passive stretching prevents the fascia from relaxing too much, one of the reasons plantar fasciitis stiffens and causes so much pain first thing in the morning. If you have had plantar fasciitis pain for longer than six months, your doctor may prescribe a night splint. It usually takes one-to-three months sleeping with a night splint for the fascia to heal. Though it can be effective in stubborn cases of plantar fasciitis, it is not exactly comfortable to sleep in a night splint.
EXERCISES AND STRETCHES TO TREAT PLANTAR FASCIITIS…AND KEEP IT FROM COMING BACK
Proper stretching is a major part of treatment for plantar fasciitis. Stretching helps strengthen not only the fascia, but the calf muscles and Achilles tendon too. Even after symptoms of plantar fasciitis resolve, it’s important to keep doing exercises to prevent a reoccurrence of the painful condition.
- Heel Raises. Stand on the edge of a step with your toes on the step and heels hanging off the end. Drop your heels down and hold for 10 to 20 seconds, then raise back up to the start position. Repeat three times (or up to 10 times as you get stronger), a few times a days. Brace yourself on a bannister, wall, or chair for balance, if needed. You will feel the stretch in your Achilles tendon and calf.
- Towel Stretch. Sit up in bed or on a mat with your legs straight in front of you. Place a rolled towel or looped necktie around the ball of one foot, holding the two ends with each hand. (You can bend the opposite knee.) Gently pull the foot toward you, keeping the leg straight. Hold the stretch for 15 to 30 seconds. Repeat five times. Switch feet.
- Marble or Dice Pickup. Sit in a chair with both feet flat on the floor and place 10 to 20 marbles on the floor in front of you. Use your toes to pick up one marble at a time and set it down a few inches to the side or put in a bowl. Repeat with the other foot. You can also do this with a washcloth, picking it up and putting it down with your toes.
- Heel Cord Stretch. Stand facing a wall with one leg forward, slightly bent at the knee. Straighten the other leg behind you with the heel flat and the toes pointed in slightly. Lean forward with both heels flat on the floor, pressing your hips towards the wall. Hold for 10 to 30 seconds, relax and straighten up. Repeat 10 to 20 times, then switch legs. Keep the knee fully extended on the side being stretched and don’t arch your back.
- Ankle cross. Sit with your feet on the floor and place your ankle across the opposite thigh, foot flexed slightly. Using the hand on the same side, gently but firmly pull your toes back towards your shin until you feel a stretch along the arch. Hold the stretch for 10 to 20 seconds, then release for 10 seconds. Repeat 5 to 10 times for each foot, several times a day. To ensure you have the right stretch position, gently run your opposite fingers across the sole of your foot; the fascia ligament should feel like a firm string along the arch.
Choosing the Right Shoes for Plantar Fasciitis
Worn or poorly constructed shoes can contribute to or aggravate plantar fasciitis. You need good arch support, heel cushioning, and shock-absorbing soles to reduce pain when standing or walking. As you step, your heel hits the ground and creates significant pressure on the fascia, causing small tears to the tissue. A properly cushioned shoe absorbs this pressure, mitigating the damage to the fascia.
While suffering pain from plantar fasciitis, it’s a good idea to avoid shoes with heels that are too high or too flat. Shoes with laces and a broad toe box can provide relief from plantar fasciitis. Try a contoured, curved insole insert that gently holds your arch. Soft silicone or gel heel pads provide shock absorption by lifting up and cushioning your heel.
RUNNING & EXERCISE SHOES
A well-fitted running shoe should have a snug heel and instep, and be wide enough so your foot can move side to side but not cross the edge of the insole, squashing your little toe against the edge of the shoe. Your toes should be able to wiggle up and down with space between your largest toe and the front of the shoe. It’s especially important that the shoe bend at the point where your foot flexes because a poorly aligned flex point can cause arch pain and plantar fasciitis.
What Are the Best Inserts for Plantar Fasciitis?
While resting your foot is an important treatment for plantar fasciitis, most of us still have to be on our feet no matter how much pain we’re in. Making your shoes more comfortable with orthotic inserts can help. The best inserts provide cushioning for shock absorption, heel cups for proper alignment, and arch support to help relieve the inflammation and pain of plantar fasciitis.
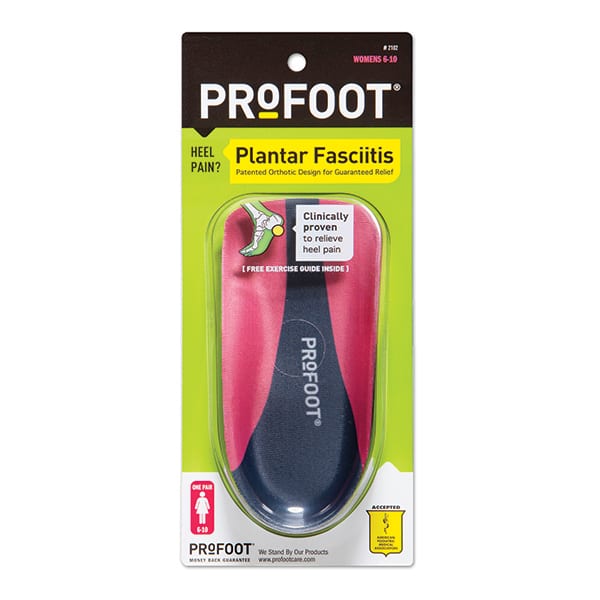
- PROFOOT Plantar Fasciitis insoles —This patented arch orthotic is designed to specifically support the entire plantar fascia and transfer pressure off of painful heels. With a deep heel cup that provides support and stability, and a gel heel insert that absorbs shock, this insert offers guaranteed relief of plantar fasciitis. Available in men and women’s sizes.
- PROFOOT Triad Orthotic—This three-quarter length insert provides 3-Zone support for heel, arch, and ball of foot. These three zones give shock absorption and relief to the balls-of-your-feet, arches, and heels to protect your knees, legs, and back. Available in men and women’s sizes.